CAR-T Cells - The Engeneered T-Cells That Are Weaponized Against Cancer
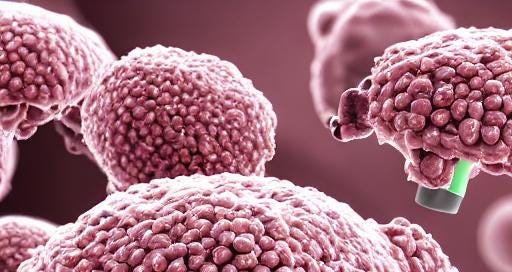
CAR-T cells, or Chimeric Antigen Receptor T Cells, represent a groundbreaking approach in the fight against cancer. These engineered immune cells are designed to specifically target tumour cells with special surface receptors, offering a new pathway for treating certain types of malignancies.
The concept behind CAR-T cells is rooted in the specificity of antigen-antibody interactions. CARs are synthetic molecular structures that detect cancer cells expressing a particular antigen, block them, and ultimately kill them. The structure of a CAR consists of four main subunits: the Ectodomain, Spacer, Transmembrane domain, and Endodomain.
The Ectodomain is the antigen-binding portion of the receptor that interacts with the epitope of the antigen. It is composed of the variable region of the light (V_L) and heavy (V_H) chain of an immunoglobulin protein, forming a single chain variable fragment (scFv). This scFv gives specificity to the receptor.
The Spacer, also known as the Hinge region, provides flexibility to the antigen-binding portion, allowing it to effectively bind with the target epitope while overcoming any steric hindrance in its path. The length of the Spacer is crucial, as its optimal length determines the CAR expression and its anti-tumor efficacy.
The Transmembrane domain is typically an alpha helix that crosses the plasma membrane, providing anchorage to the receptor. The stability of the receptor and intracellular signalling depends on the choice of the transmembrane domain.
The Endodomain is the primary focus of the CAR receptor, responsible for intracellular signalling and generating an immune response. Over time, modifications to the Endodomain have led to the engineering of four generations of CAR-T cells.
The first generation of CAR-T cells had a single structure from the intracellular domain to generate an immune response. However, it was unable to produce enough interleukin to kill cancer cells effectively. To address this, the second generation of CAR-T cells incorporated three different types of receptors on the T cell antigen receptor, including a cytokines receptor and a co-stimulatory receptor to promote interleukin production. The third generation enhanced cytokine production and killing ability by combining multiple receptors. The fourth generation, known as TRUCKs (T cell Redirected Universal Cytokine-mediated killing), was created by slightly modifying the second generation. TRUCKs are highly effective at activating immune cells and eliminating antigen-negative cancer cells in the targeted region.
Despite the promising results of CAR-T cell therapy, there are several limitations and challenges to overcome. These include antigen escape, off-target effects on normal cells, tumour infiltration, immunosuppressive microenvironment, cytokine release syndrome (CRS), T-cell exhaustion, neurotoxicity, ineffectiveness against solid tumours, and high costs.
Nevertheless, CAR-T cell therapy has revolutionized cancer treatment, showing unexpected results in clinical trials and gaining approval from the US Food and Drug Administration (FDA). For instance, the first CAR-T drug, Tisagenlecleucel, used in B cell lymphoma patients, resulted in a 58% complete response with an 82% overall response.
In conclusion, while CAR-T cell therapy brings new hope for people suffering from certain haematological
malignancies, there are still many side effects and future challenges to deal with. Ongoing research aims to improve these immune cells, and once all modifications are made, we can expect that it will be an effective cure against cancer. However, it is too soon to say that CAR-T cells can completely cure cancer.